Alliance Update: Here’s summary of NY’s New 1115 Medicaid Waiver agreement by former NYS Medicaid Director Jason Helgerson, Greg Allen, Kailin Scott and Juliette Price.
Everything You Need to Know about New York’s Newly-Approved $6B Medicaid Waiver
This post was jointly written by Jason Helgerson, Founder & CEO, Juliette Price, Chief Solutions Officer, Greg Allen, Senior Advisor, and Kalin Scott, Senior Advisor.
Helgerson Solutions Group
NY’s new waiver doubles down on the provision of health related social needs, hospital global budgets, and workforce investments. Don’t have the time to read the 239 pages of details?
After much anticipation, negotiation with the federal government, whispers about what’s in and what’s out, New York State’s new Medicaid 1115 waiver is here, in its final, approved form in partnership with the Centers for Medicare and Medicaid Services (CMS) and New York State Department of Health (DOH).
Down from the state’s original $13 billion request submitted in September of 2022, this $6 billion waiver focuses on advancing health equity, reducing health disparities, supporting the delivery of health-related social services, and promoting workforce development. The waiver period formally begins in April 2024 is set to expire March 31, 2027, giving New York just 3+ years to implement this ambitious program.
The Basics:
The main components of the waiver program are:
- Health related social needs services and activities
- Medicaid Hospital Global Budget Initiative
- Workforce investments
- Establishment of a Health Equity Regional Organization (HERO)
- Alignment to two CMMI alternative payment models.
Each of these program components is broken down in detail in this post.
The stated goals that CMS and New York State are agreeing to accomplish are:
- Investments in HRSN via greater integration between primary care providers and community-based organizations (CBOs) with a goal of improved quality and health outcomes;
- Improve quality and outcomes of enrollees in geographic areas that have a longstanding history of health disparities and disengagement from the health system, including through an incentive program for safety net providers with exceptional exposure to enrollees with historically worse health outcomes and HRSN challenges;
- Focus on integrated primary care, behavioral health (BH), and HRSN with a goal to improve population health and health equity outcomes for high-risk enrollees including kids/youth, pregnant and postpartum individuals, the chronically homeless, and individuals with SUD;
- Workforce investments with a goal of equitable and sustainable access to care in Medicaid; and
- Develop regionally focused approaches, including new VBP programs, with a goal of statewide accountability for improving health, outcomes, and equity.
What’s Being Prioritized in this Waiver?
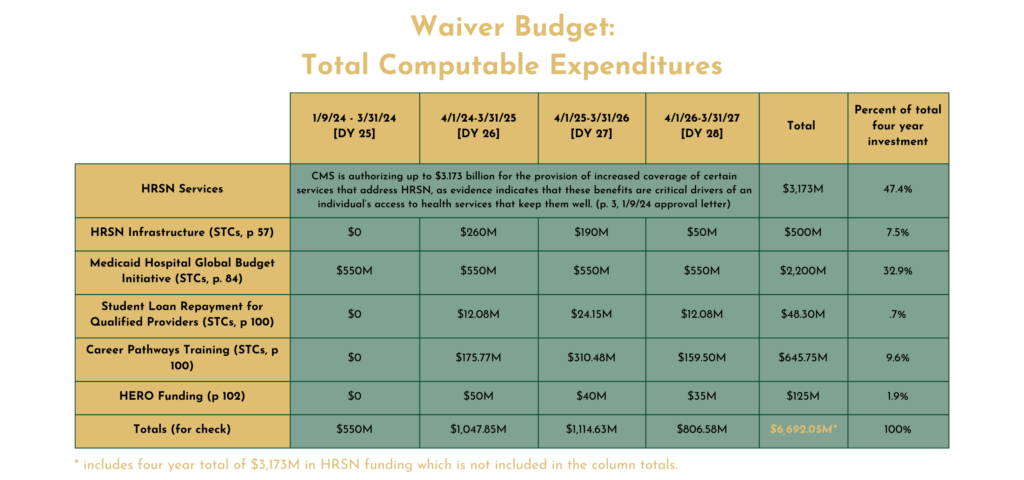
As the age-old saying goes, “Show me your budget, and I’ll show you your priorities.” To that end, we’ve pulled together a summative budget chart that shows where the funding is being prioritized.
Nearly half (47%) of the budget is allocated towards the provision of health related social need services, with 33% of the budget going towards the Medicaid Global Hospital Budget Initiative. Rounding out third with 10%+ of spending is the workforce development activities, followed by investments in the health related social needs infrastructure building, and lastly 2% towards the creation of a statewide HERO.
The details of each of these program components can be found below in the blog post.
HIGH LEVEL WAIVER TAKEAWAYS
Here are some of the key 60,000-ft reflections our team had to the wavier as a whole:
How much “new” money does the waiver represent? We don’t know for sure and it would be great if NYS DOH provided some clarity on this question. Official press releases suggest $6 billion in new federal funding, but the math is still a bit murky. Buried in the document is also a specific cap on the use of Designated State Health Programs (DSHP) as a source of local match ($3.98 billion) and a requirement that the state contribute general tax dollars to the effort. All this suggests that while the state may have the authority to claim up to $6 billion in new federal funding, it may need to find hundreds of millions of state tax dollars to achieve that level of federal investment. If that is the case, the state’s current difficult budget situation may lead to a smaller-than-anticipated program.
This new program isn’t DSRIP 2.0. New York’s last 1115 Waiver program, known as DSRIP, was all about accountability and pay-for-performance. It ensured that the state and associated participating organizations wanted to access federal funding made available through the waiver, it had to earn it through measurable improvement in patient outcomes. None of the federal funding in this program is tied directly to performance and there is no statewide report card. This new effort is more about covering additional services, funding struggling hospitals, and implementing some additional smaller, stand-alone programs. The biggest opportunity in the waiver is to expand the Medicaid program to formally include payment for health-related social needs services that are vital to addressing the social care needs of Medicaid members.
The program commits NY to AHEAD and Hospital Global Budgets. For better or worse, the waiver commits New York to hospital global budgets. As much as $2.2 billion will be available for non-profit, financially distressed hospitals in Brooklyn, Queens, Bronx, and Westchester Counties–but the price of those funds will be participation in hospital global budgets. Hospital global budgets are controversial because they lock savings generated by efforts to reduce avoidable hospital use into the four walls of hospitals and prevent those funds from being reinvested in primary care or community-based behavioral health services. That said, global budgets could make it easier for hospitals to restructure and allow them to be more sustainable long-term. No matter where opinions falls in this debate, the waiver puts New York on a path toward hospital global budgets in at least one part of the state.
NYS is looking for a HERO. The waiver includes modest funding for the establishment of a single, statewide Health Equity Regional Organization (HERO). This organization will be tasked with population health improvement efforts with a special focus on identifying and addressing health disparities. This organization will also help advise the state as it looks to further value based payment efforts across the state. The state’s original proposal envisioned multiple regional HEROs, but ultimately CMS was only willing to fund a single, statewide entity. Sounds like we’re looking for a superhero, more than just a hero.
Significant workforce investment. More than $690 million will be invested in the state’s health care workforce and efforts to bring sustainability to the workforce challenges being acutely felt today. Specifically, the waiver creates two programs designed to expand and enhance the state’s healthcare workforce. Workforce Investment Organizations (WIOs) will have a major new responsibility under this program because they will take the lead in implementing the Career Pathways Training (CPT) program. CPT will target workforce shortages in healthcare staffing, support the delivery of HRSN services, and increase access to culturally appropriate services. WIOs were created under the last 1115 waiver and will once again play a key role in workforce initiatives funded by a Medicaid waiver.
No investment in Long-Term Care. Even though long-term care (LTC) is the biggest cost driver in New York’s Medicaid program, the waiver fails to allocate any specific funding or programs to the population that receives those services. It is worth noting that LTC recipients could very well benefit from the health-related social needs services created under the waiver. That said, there isn’t specific funding for LTC providers. The last 1115 waiver focused its workforce funds on LTC, but this newest round of workforce funding is more about helping to prepare the health related social needs workforce as opposed to up-skilling LTC workers. Missed opportunity or an appropriate omission? The answer is in the eye of the beholder.
Implementation will be a huge challenge. NYS DOH is facing a huge implementation challenge with this new waiver. While the last Medicaid waiver ushered in a 6-year program, the new waiver is only 3.5-4 years in duration, depending on how you count the money. To implement, the state will need to conduct multiple, complex procurements in addition to training thousands of organizations across the state on what new services will be funded and how to bill for those services. Other states have struggled to implement waivers with programs similar to this one and hopefully, NYS will have learned from those struggles. Also worth noting is that no administrative funds are being made available to help DOH implement the waiver programs–the last waiver provided DOH with a significant pot of funds which was essential for hiring staff and consultants to help with a complex implementation. Unfortunately, there are no such additional resources in this waiver amendment.
PROGRAM COMPONENTS: WHAT MAKES UP THIS WAIVER PROGRAM?
Health Related Social Needs (HRSN)
The waiver advances a significant statewide effort to promote health equity, reduce health disparities and improve quality through the provision of services to address Health Related Social Needs (HRSN). Contracted through managed care plans, Social Care Networks (SCNs) are the primary entities that will organize HRSN programming delivered primarily by local social care providers. The HRSN is the flagship effort in the waiver with almost half of total computable dollars dedicated to the provision of social care, primarily to high risk populations.
HRSN infrastructure–meaning the creation of the SCNs–will be built on a regional basis, with one entity in each of the state’s regions. $500 million has been allocated for this infrastructure build, with the bulk of that investment happening in early demonstration years and ramping down from there. The state will use a procurement process to select the SCNs. Expect this process to be brutally fast and highly competitive.
HRSN services are targeted to a waiver-limited population set based on the two levels of service described below. The state may further limit target populations and services in its federally required delivery plan, which is yet to be completed and approved. HRSN service providers must match the member’s clinical and medical needs based on medical appropriateness established using standardized criteria. HRSN services delivered under the waiver must have a reasonable expectation of improving or maintaining the health or overall functioning of the member.
Service Levels
- Level One Services
- Screening
- Level One Case Management – navigation to state, federal, and local HRSN programs outside of the 1115 demonstration to address HRSN needs
- Members can be in FFS or Managed Care and don’t need to be in the higher risk target populations eligible for Level Two services
- Level Two Services
- Case Management
- Housing
- Nutrition
- Transportation
- Members must be enrolled in Medicaid Managed Care AND be in the higher risk target populations described below
For Level Two services, members must be in one of the following target populations and be individually assessed for medically needing HRSN services based on forthcoming state-submitted and CMS approved criteria:
- Eligible Target Populations for Level Two Services (must also meet clinical criteria)
- Medicaid high utilizers (defined by inpatient, ED or total Medicaid spend and/or meeting federal homelessness criteria)
- Individuals enrolled in NYS Health Home (includes multiple chronic conditions)
- Individuals with SUD
- Individuals with SMI
- Individuals with Intellectual and Developmental Disabilities
- Pregnant persons, up to 12 months postpartum
- Post-release criminal justice-involved population with serious chronic conditions, SUD, or chronic Hepatitis-C
- Juvenile justice involved youth, foster care youth, and those under kinship care
- Children under the age of six
- Children under the age of 18 with one or more chronic conditions
Other HRSN details:
- The state has to submit a plan to CMS for how it will utilize waiver infrastructure dollars to set up HRSN services, which evidence-based HRSN services it will cover, how it will select and qualify providers, how it will screen and qualify members, how it will develop and implement standardized clinical criteria for HRSN services, how it will develop HRSN rates and how it will coordinate with and not duplicate existing HRSN services such as those delivered by SNAP and WIC
- HRSN services start out being paid on a non-risk basis but the state will move them to payment on a risk basis no later than April 1, 2027.
- HRSN services have to be claimed using standardized claims and encounter reporting.
- Managed care plans will contract with SCNs to organize and deliver HRSN services.
- SCNs must establish a network of qualified social service providers to deliver HRSN services.
- Social Service Providers do not need to be licensed for HRSN services unless the specific service requires a license.
- Managed care plans will pay providers state set rates for HRSN services.
- Managed care plans are responsible for assuring HRSN network capacity and member voluntary access to HRSN services. Plans can’t use HRSN services to reduce, discourage, or jeopardize Medicaid beneficiaries’ access to other Medicaid covered services.
- In a performance report to CMS, the state must report on beneficiary HRSN participation, screening, rescreening, receipt of referrals, recurring nutrition services, and social services over time, along with other items.
Key takeaways:
- It is clear that health care quality and efficiency, especially for higher risk members, require that social determinants of health be addressed. Aiming bigger dollars at an HRSN service build is directionally spot on. The challenge here is likely to be the scale of this undertaking with the time allotted to get the dollars out the door. Especially given downstream workforce challenges that the social sector faces in every community in New York.
- The state’s relatively recent experience with building new services under modified HCBS waivers was that even when providing semi-attractive Medicaid rates for new services, providers are so busy keeping the lights on that new services are very hard to scale. Will this be as true for social care providers as it has been for clinical providers? We will see. HCBS was complicated and rules were tight. Conversely, the framework here (so far) is fairly broad and perhaps this wiggle room combined with the relatively large number of social care providers (most without a built FFS revenue stream) will speed up the scale here (deep apologies to DSRIP survivors for using both speed and scale in the same sentence).
- The other challenge, assuming a broad launch of HRSN services, could be transitioning and maintaining these new services in a risk-based managed care model. Will these new services be valued by the plans? In a constrained fiscal environment, how much money will remain in capitation rates to cover these services after the expiration of the waiver? How much of the “value” in value based payment can be attributed to the addition of these “new” services? Perhaps a robust effort to measure ROI by HRSN service grouping and member risk group will help all begin to understand these services’ impacts on both quality and cost.
MEDICAID HOSPITAL GLOBAL BUDGET
One of the biggest policy components of the new waiver is a commitment to hospital global budgets. CMMI recently announced a new demonstration program called Advancing All-Payer Health Equity Approaches and Development (the AHEAD model) which aims to expand the use of multi-payer hospital global budgets beyond their current implementation efforts, which include Maryland, Vermont, and a portion of Pennsylvania. Proponents of the approach believe that it allows hospitals to transform care and shift resources from inpatient services to the outpatient environment. Opponents feel that it has the potential to create a permanent institutional bias in the health care ecosystem by permanently locking in hospital spending that is avoidable and should rather be spent in community settings.
The new waiver specifically creates the Medicaid Hospital Global Budget Initiative in New York, aiming to provide financial support to certain hospitals in specific counties to improve quality of care and promote alternative payment models. The state can receive $2.2 billion over four years, with annual payments of $550 million, contingent on meeting specified criteria.
Eligible hospitals must be private not-for-profit hospitals in designated counties (Bronx, Kings (Brooklyn), Queens, and Westchester) with a Medicaid and uninsured payor mix of at least 45%. They should also have an average operating margin of 0% or less over the past four years and must have received state-only subsidies due to financial distress in specified fiscal years.
Key takeaways: The devil is in the details around any global budget model, and at this point the details are scarce. We know the state must submit a plan to implement a Medicaid Hospital Global Budget Model, either through participation in the AHEAD model or by submitting its own Medicaid Hospital Global Budget methodology. The plan will need to include details on services covered, budget construction, updates, quality improvement strategy, and health equity initiatives. The exact method for calculating or changing global budgets is a giant TBD. There is also have no clarity on how these budgets will interface with other Medicare and Medicaid alternative payment model programs such as the Medicare Shared Savings Program (MSSP), ACO REACH, and New York’s Medicaid VBP Innovator Program. Everyone should closely watch this effort as it could have major implications for existing value based payment efforts across New York City, and ultimately New York State.
============
WORKFORCE INVESTMENTS
In support of the overall waiver goals to address health disparities, promote health equity, and support investments in addressing the health-related social needs of Medicaid members, the state will invest more than $690 million in workforce initiatives. The investments aim to strengthen the health care workforce by addressing existing provider shortages and funding training and education opportunities to create a reliable health care workforce pipeline.
A total of $48.3 million will fund student loan repayment for certain types of providers in exchange for a multi-year commitment to work with Medicaid members. Psychiatrists, primary care physicians, dentists, nurse practitioners, and pediatric clinical nurse specialists will be eligible for the Student Loan Repayment for Qualified Providers program. After being selected through a competitive state-run application process, eligible providers are required to make a 4-year commitment to maintain a patient panel that includes at least 30% Medicaid or uninsured patients.
Workforce Investment Organizations (WIOs)–created as part of the state’s MRT Waiver Amendment to support training for the long-term care workforce–will leverage their expertise to implement, manage and provide oversight of the $645.75 million Career Pathways Training (CPT) program. Current health care workers accepted into eligible training and education programs can apply to participate in the Healthcare Career Advancement Pipeline. Individuals who are unemployed or do not work for a health care provider are eligible to apply to the New Careers in Healthcare Pipeline. Participants in both pipelines will commit to 3 years of service in their new professional title, working for New York health care providers enrolled in the Medicaid program that serve at least 30% Medicaid members and/or uninsured patients.
Eligible training and education programs will include the following:
- Nursing titles (Licensed Practical Nurse, Associate Registered Nurse, Registered Nurse to Bachelor of Science in Nursing, Nurse Practitioner)
- Professional technical titles (Physician Assistant, Licensed Mental Health Counselor, Master of Social Work, Credentialed Alcoholism and Substance Abuse Counselor, Certified Pharmacy Technician, Certified Medical Assistant, Respiratory Therapist)
- Frontline public health workers (Community Health Worker, Patient Care Manager/Coordinator)
Key Takeaways: This isn’t the first time that New York has recognized the importance of funding Medicaid workforce training, recruitment, and retention efforts aligned with its strategic vision. The state clearly saw the value and benefit of these efforts in the last 1115 waiver, including the MLTC Workforce Investment Program, the creation of WIOs, and the benefit of aligning workforce training with population health and value-based payment objectives. This new waiver funding builds on that infrastructure, expands beyond long-term care, and will be an integral component in addressing the health and social care needs of the state’s Medicaid members.
HEALTH EQUITY REGIONAL ORGANIZATION (HERO)
A smaller investment, but a very large job, awaits the HERO–Health Equity Regional Organization–described in the new waiver. With just $125 million (total computable) over the demonstration period, this single entity will be responsible for designing regionally-focused approaches to reducing health disparities, advancing quality and health equity for overall populations, and supporting the delivery of health related social need services.
The HERO’s main activities will include:
- Data aggregation, analytics, and reporting: statewide data crunching that will include data submitted by managed care organizations, social care networks, workforce investment organizations, provider-submitted data; integrating health and social data set (best wishes to the HERO on this one, not many nationally have cracked this nut); evaluate the needs/gaps in access to physical/behavioral/social care.
- Conducting regional needs assessment and planning: this organization will conduct annual regional planning, write a statewide health equity plan, and make sense of the workforce-related shortages and needs.
- Convene regional stakeholder engagement sessions: no more detail than this.
- Make recommendations to support advanced value-based arrangements and develop options for incorporating health related social need services into value based payment methodologies: the state is looking to outsource the creation of new value based payment methodologies for them to start using at the end of the demonstration period, with specific focus on how to pay for health related social needs moving forward.
- Conduct program analysis, such as publishing initial health equity plans and health factor baseline data on Medicaid populations.
New York is seeking a real unicorn here, and has specifically required that this be an independent actor from the state or other government entities.
Key Takeaway: This is an incredibly large policy role to be handing over to a non-state actor. In fact, when one reads the main descriptions of what the HERO will be responsible for, one may find oneself asking “Isn’t that DOH’s job?” Additionally, fulfilling this role will require deep expertise in lots of areas–approaches to health equity, data acquisition, cleaning, organizing and analytics, and dissemination, not to mention the development of new, cutting-edge value based payment models. It sounds like too much expertise for one organization alone to fill, so we may see the HERO eventually be a conglomerate of multiple organizations or actors.
WHAT OTHER PRIORITIES FOUND THEIR WAY INTO THE WAIVER?
Mandatory Provider Rate Increase
The new waiver demonstrates CMS’s clear intent to use 1115 waivers to drive up reimbursement for essential services. CMS has required increases of this type in other states and New York is no different. Specifically, as a condition of waiver approval, New York will increase and subsequently sustain Medicaid fee-for-service provider base rates for a specific set of services. In addition, the state will need to mandate that its Medicaid Managed Care plans implement the same rate increases for eligible providers.
The rate increases will be at least two percentage points in the ratio of Medicaid to Medicare provider rates for one of the service categories that comprise the state’s definition of primary care, behavioral health care, or obstetric care, as relevant, if the average Medicaid to Medicare provider payment rate ratio for a representative sample of these services for any of these three categories of services is below 80 percent. This requirement can apply to single delivery systems within each service category if the Medicaid:Medicare ratio is only below 80 percent in either FFS or MMC. New York is additionally required to invest $199,072,125 (total computable) in rate increases as part of the demonstration amendment, which must be sustained by the state once implemented.
The state investment is required even if no Medicaid rates are below 80 percent of Medicare rates. The state may make the rate increases in any demonstration year, but the net provider rate increases must amount to $199,072,125 by the end of the demonstration period. The state may not decrease provider payment rates for other Medicaid or demonstration covered services to make state funds available to finance provider rate increases (i.e., cost-shifting).
Key Takeaways: First, CMS is trying to create a formal link between Medicare and Medicaid reimbursement–CMS fears that Medicaid rates are falling behind Medicare rates, which is leading to access challenges and so CMS is using its leverage with New York to create a more formal link. This could lead the state to implement additional rate increases in the future.
Second, this creates a powerful Maintenance of Effort (MOE) that could protect provider rates over the next several years. New York State won’t be allowed to cut Medicaid provider rates or risk violating the MOE which in turn would put federal waiver funds at risk. This MOE should be seen by providers as very good news as we enter what looks to be a difficult budget environment.
Substance Use Disorder Services
In December, the state requested demonstration authority to draw in federal funds for previously non federally-eligible residential Substance Use Disorder (SUD) services in facilities the federal government calls “Institutions for Mental Diseases” or IMDs. CMS has offered states a pathway to bring in new federal funds to pay for these previously non-federally eligible services if states agree to also provide a full range of services to address SUD. Although New York’s request was separately submitted, CMS is approving the SUD IMD demonstration concurrent with the rest of this waiver.
A Health Information Technology plan specific to SUD is implemented as part of the waiver to advance care coordination, prescription monitoring and quality improvement, among other aims.
Goals of the new SUD Implementation plan include:
- Increase rates of identification, initiation, and engagement in treatment for SUD
- Increase adherence to and retention in treatment
- Reduce overdose deaths, particularly those due to opioids
- Reduce utilization of emergency departments and inpatient hospital settings for treatment where the utilization is preventable or medically inappropriate through improved access to other continuum of care services
- Fewer readmissions to the same or higher level of care where the readmission is preventable or medically inappropriate
- Improve access to care for physical health conditions among beneficiaries with SUD
For the SUD program, the state must include an assessment of the objectives of all components of the demonstration. Hypotheses may include compliance with treatment, utilization of health services (emergency department and inpatient hospital settings), and a reduction in key outcomes such as deaths due to overdose.
Key Takeaway: The SUD authority granted in the waiver will allow Medicaid members to have access to a fuller continuum of evidence-based Opioid Use Disorder/Substance Use Disorder treatment services under standardized placement criteria including access to services delivered in newer community based settings.
Continuous Eligibility for Children
A little-known fact outside of Medicaid-land is that nearly half of all Medicaid members nationally are children (and that children really are, indeed our future). This population has been a focus of the Biden-Harris Administration, especially through the unwinding of the Public Health Emergency (PHE) related to Covid-19, to ensure that children do not lose their access to health insurance. In general, children are low-cost beneficiaries on the program, with approximately 2% of this population being medically complex and costly.
Recently approved 1115 waivers in other states have specifically included Continuous Eligibility for Children programs, which means that children under the age of 6 are not required to reapply (or be redetermined) for Medicaid eligibility after first-time approval for the program. This is important because we know that parents are busy raising their children, working, and managing the daily stresses of life, so allowing continued coverage for kids up to age 6 reduces the likelihood that health care services are denied to children over a missed deadline for re enrollment. The PHE unwinding data has also shown that an inability to reach parents for re enrollment often leads to kids being dropped from the program. This continuous eligibility program will ensure kids stay covered, even if parents are not.
In the document released with the waiver details, CMS outlines that the continuous eligibility for children program is not technically included in this waiver, but that New York State has stated intention to CMS to submit an amendment in early 2024 to include the program.
Key takeaway: Children under six represent one of our nation’s most valuable resources–they are in their key development phases, and access to preventative care can significantly increase their likelihood of success, against health, academic, and social measures. It’s one of the best investments our country can make at an incredibly low cost to taxpayers–in fact, its when we don’t invest early that costs balloon later on.
ALIGNMENT WITH CMMI ALTERNATIVE PAYMENT MODELS
Since Medicaid is a state-federal partnership, it is to be expected that CMS seeks to align this waiver with its other portfolio programs. Most notably, this waiver aligns with CMMI’s alternative payment models: the AHEAD Model and the Making Care Primary Model.
New York State is aligning itself with the AHEAD Model, through the commitment to a Medicaid Global Hospital Budget Program. See the above section for details.
New York State also aligned itself with the Making Care Primary model, released earlier in 2023. MCP is a Medicare program that centers primary care providers and provides a glidepath to value based arrangements through capitation payments for primary care. In the waiver document, New York’s alignment to MCP is vaguely referenced, in a section where CMS details that New York requested authority from CMS to direct its managed care plans to make Medicaid Patient Centered Medical Home (PCMH) payments align with the PCMH payments available to providers through the Medicare MCP model. CMS simply states that New York does not need section 1115 authority to direct the managed care plans to do so, and that New York State intends to pursue State-Directed Payment authority for these payments in the future.
Key Takeaways: It’s clear that DOH is working to align Medicaid PCMH payments with the Making Care Primary PCMH Payments, through the managed care plans, but no other details about the alignment to Making Care Primary is included. This will be a space to watch for providers.
About the Authors: This post was jointly written by Jason Helgerson, Kalin Scott, Greg Allen and Juliette Price Helgerson Solutions Group
https://www.hsg.global/insights/1115-medicaid-waiver-approved-what-you-need-to-know