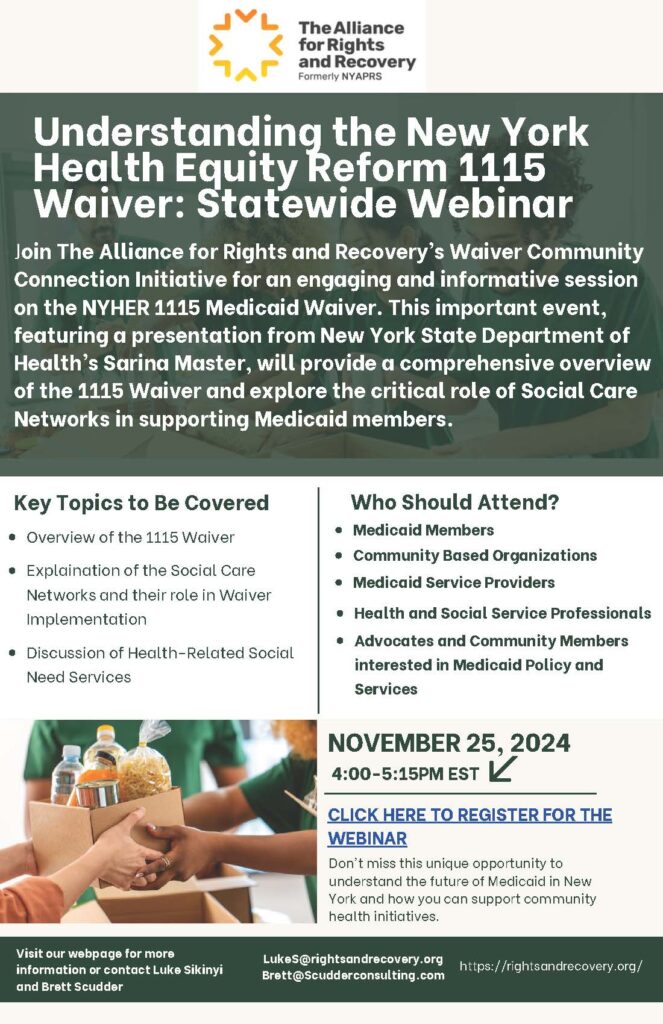
Alliance Alert: Don’t Miss the Alliance’s timely and informative webinar on the New York Health Equity Reform (NYHER) 1115 Medicaid Demonstration Waiver next Monday (11/25) afternoon, from 4-5:15pm! We’re pleased to offer presentations from Sarina Master, Director of Adult Special Populations, Policy and Programming at the New York State Department of Health (DOH) Harvey Rosenthal, CEO of The Alliance for Rights and Recovery, Brett A Scudder, and Luke Sikinyi along with representatives from the Office of Mental Health (OMH).
Background:
Medicaid Demonstration Waivers are a tool to test funding for services typically not covered by Medicaid. These waivers are used by states to prove the effectiveness of offering new services in improving people’s health and lives. New York’s new 1115 Waiver aims to reduce health disparities, such as lessor access to healthy foods among people in low-income communities. The Waiver aims to coordinate health related social need services, which are supports for social needs which have an affect on people’s health such as providing packaged healthy meals for Medicaid members, through the new Social Care Networks.
These networks are groups of providers who are connected through and working under a lead agency to coordinate and provide services to eligible people. While the waiver is complex, our upcoming webinar will help you gain a better understanding of how the Social Care Networks work and what Medicaid members looking for additional services should expect.
See below for more information, including a link to register for the webinar and a brief overview of the 1115 Waiver goals.
More Information on the Waiver
The NYHER 1115 Medicaid Demonstration Waiver represents a transformative effort by New York State, in partnership with the Centers for Medicare & Medicaid Services (CMS), to advance health equity, reduce health disparities, and address social determinants of health (SDOH). This initiative will leverage $7.5 billion in funding over three years to implement innovative programs aimed at improving health outcomes for Medicaid recipients.
Key goals of the waiver include:
- Addressing Health-Related Social Needs (HRSNs):
- Establishing Social Care Networks (SCNs), which aregroups of local providers who are connected within a system to coordinate and provide needed health services for such as housing support, nutrition assistance, and transportation for Medicaid members
- Integrating behavioral health, primary care, and social services to ensure holistic care delivery for underserved communities.
- Advancing Health Equity:
- Reducing disparities in care for children, pregnant and postpartum people, and high-risk adults by expanding access to culturally appropriate and community-driven services. Examples of health disparities include less access to healthy foods among people in low income communities or less access to effective mental health supports for communities of color.
- Supporting safety net hospitals that serve populations with the greatest health needs by ensuring sustainable funding and transitioning to value-based payment models.
- Expanding Behavioral Health Services:
- Enhancing access to comprehensive, coordinated treatment for substance use disorders (SUDs).
- Improving integration between behavioral health and primary care providers to better serve Medicaid populations.
- Strengthening the Healthcare Workforce:
- Addressing critical workforce shortages by creating career pathways training programs for frontline health and social care professionals.
- Launching a loan repayment program to incentivize clinicians, including dentists and psychiatrists, to work in underserved areas.
- Supporting peer-led workforce development to integrate individuals with lived experiences into the delivery of recovery services for mental health and substance use care.
- Investing in Primary Care:
- Developing a “Making Primary Care Primary” initiative to strengthen primary care infrastructure.
- Aligning Medicaid and Medicare value-based payment strategies to improve population health outcomes.
- Facilitating Community-Based Organization (CBO) Integration:
- Allocating $500 million to SCNs to build infrastructure and empower CBOs to deliver Health-Related Social Need (HRSN) services.
- Ensuring CBOs have the necessary support and resources to partner effectively with SCN leads, emphasizing their critical role in community service delivery.
- Promoting Value-Based Care:
- Advancing the transition to value-based contracting to prioritize quality over quantity in care delivery.
The waiver reflects New York’s commitment to creating a more equitable and integrated healthcare system that prioritizes prevention, holistic care, and sustainable solutions to long-standing health disparities. Continued advocacy and support for community-based providers and individuals with lived experiences will be critical to ensuring the success of these ambitious goals.