Quick Links
- General Background
- How the Waiver Will Work
- Find Your Social Care Network
- For Medicaid Members
- For Community-Based Providers and Organizations
- Services Funded Under Waiver
- View the Screening Questionnaire
- Career Pathways Training Program
- Frequently Asked Questions
- Past Events and Materials
- Submit Your Questions
The Waiver Community Connection Initiative, led by the Alliance for Rights and Recovery, supports New York’s 1115 Medicaid Waiver to reduce health disparities and improve health equity. These disparities—such as higher illness rates or lower life expectancy—stem from social, economic, and systemic inequalities.
The waiver emphasizes Social Determinants of Health (SDOH)—the conditions where people live, learn, and work—by shifting focus from medical services alone to addressing Health-Related Social Needs (HRSNs), which are immediate individual barriers to health.
The initiative prioritizes education, empowerment, and engagement. By educating Medicaid members and community organizations through webinars, forums, and peer-led activities, it fosters informed participation and enables people to shape local mental health and social care systems.
This collaborative approach amplifies community voices, strengthens local services, and promotes improved health outcomes and equity across New York.
General Background on Waiver
The New York Health Equity Reform Medicaid Waiver
What does it mean for medicaid members and community-based providers?
Beginning in January 2025, community-based agencies (CBOs) and providers will begin conducting “health-related social needs” assessments of all Medicaid members.
Based on the results of the assessments, referrals can be made to services and supports that match each person’s needs.
For Medicaid members in managed care programs, health related social need services can be offered to assist with housing, food, transportation, and case management. For example, people who have food insecurities may receive healthy packaged meals delivered.
Social Care Networks will manage the overall system to document every assessment and referral. The goal is to measure outcomes to determine how social supports can improve health care.
The NYHER 1115 Medicaid Demonstration Waiver represents a transformative effort by New York State, in partnership with the Centers for Medicare & Medicaid Services (CMS), to advance health equity, reduce health disparities, and address social determinants of health (SDOH). This initiative will leverage $7.5 billion in funding over three years to implement innovative programs aimed at improving health outcomes for Medicaid recipients.
Key goals of the waiver include:
- Reducing disparities in care for children, pregnant and postpartum people, and high-risk adults by expanding access to culturally appropriate and community-driven services. Examples of health disparities include less access to healthy foods among people in low income communities or less access to effective mental health supports for communities of color.
- Supporting safety net hospitals that serve populations with the greatest health needs by ensuring sustainable funding and transitioning to value-based payment models.
- Enhancing access to comprehensive, coordinated treatment for substance use disorders (SUDs).
- Improving integration between behavioral health and primary care providers to better serve Medicaid populations.
- Addressing critical workforce shortages by creating career pathways training programs for frontline health and social care professionals.
- Launching a loan repayment program to incentivize clinicians, including dentists and psychiatrists, to work in underserved areas.
- Supporting peer-led workforce development to integrate individuals with lived experiences into the delivery of recovery services for mental health and substance use care.
- Developing a "Making Primary Care Primary" initiative to strengthen primary care infrastructure.
- Aligning Medicaid and Medicare value-based payment strategies to improve population health outcomes.
- Allocating $500 million to SCNs to build infrastructure and empower CBOs to deliver Health-Related Social Need (HRSN) services.
- Ensuring CBOs have the necessary support and resources to partner effectively with SCN leads, emphasizing their critical role in community service delivery.
- Advancing the transition to value-based contracting to prioritize quality over quantity in care delivery.
The waiver reflects New York’s commitment to creating a more equitable and integrated healthcare system that prioritizes prevention, holistic care, and sustainable solutions to long-standing health disparities. Continued advocacy and support for community-based providers and individuals with lived experiences will be critical to ensuring the success of these ambitious goals.
Watch DOH’s Waiver Amendment Overview Presentation here: NYHER 1115 Waiver Amendment Overview (YouTube) - February 21, 2024
How the Waiver Will Work

The waiver allows New York to use Medicaid funds to address “health-related social needs,” specifically, temporary support for housing, food, transportation and case management.
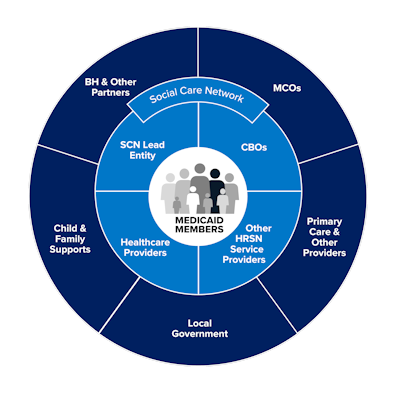
To coordinate the delivery of these services, the state has been organized into nine geographic areas, called Social Care Networks, each with a Lead Entity responsible for developing a comprehensive network to screen all Medicaid members for social needs.
Find Your Social Care Network
From DOH: The establishment of Social Care Networks (SCNs) is a core part of the NYHER Amendment. New York State has established 9 regional Social Care Network Lead Entities who are responsible for building a robust Network of Community-Based Organizations (CBOs) and other organizations providing health-related social needs services and coordinating with health care providers (inclusive of behavioral health and primary care providers). Together, each Social Care Network is responsible for ensuring that there is a seamless, consistent, coordinated, end-to-end process in their region for Screening, Navigation, and delivery of health-related social needs services. This requires close collaboration within each Network, as well as shared data and technology provided by the State. Social Care Network Lead Entities also engage a broader ecosystem of partners to achieve their goals, including health insurance plans, local government, and child & family supports.
For Medicaid Members
For Individuals Who are Enrolled in Medicaid Managed Care
For Medicaid members in managed care programs, “enhanced” health-related social needs services can assist with housing, food, transportation, and case management. For example, healthy packaged meals may be delivered for up to six months to individuals experiencing food insecurity.
To be eligible for this extra support, you need to complete a special social needs assessment survey. The survey can be administered by a CBO or provider you work with already, or you may complete the survey yourself on the website of your regional Social Care Network. Contact information for the networks can be found here in the tab labeled “Find Your Social Care Network.” Beginning January 1, 2025, your managed care program is supposed to share your contact information with your regional social care network.
For Individuals Who are on Regular Medicaid
Medicaid recipients not enrolled in a managed care plan may also be assessed for health-related social needs but cannot access enhanced service. Instead, they can receive case management support to connect with existing community-based services that match their needs.
For Community-Based Providers and Organizations
Each SCN is responsible for recruiting community-based organizations and providers within their jurisdiction to screen Medicaid members for health-related social needs and connect them to eligible support services. This process began in August 2024 and is continuing in most regions.
For CBOs and providers, it’s essential that you contact the Lead Entity for your region to learn how the service is going to function and decide whether or not to join the network. A list of contacts for each region can be found here.
To assist providers in understanding exactly what services can be delivered and the payment for that work, we have created a simplified list of each service and the corresponding time allotted for billing purposes. You can find this list in the section below, labeled “Services Funded Under Waiver.”
From the NYS Department of Health:
The Social Care Network program brings new or expanded opportunities for providers of nutrition, housing, transportation, and social care management services. Organizations that provide at least one health-related social needs service can join a Social Care Network. Joining a Social Care Network means contracting with one or more Lead Entities and participating in required trainings. Organizations spanning multiple regions may contract with multiple Social Care Network Lead Entities. Reach out to the Lead Entity in your region(s) to learn more.
For more information, please review the SCN: Introduction for HRSN Service Providers Guide. (PDF).
Overview of Reimbursement Processes
Health-related social needs service providers who join a Social Care Network will be paid by the regional Lead Entity for screening and/or services they deliver.
To receive reimbursement, health-related social needs service providers must:
- Be in contract with a Lead Entity (note, HRSN providers can join more than one SCN)
- Provide screening and/ or services in a manner consistent with the Social Care Network program
- Complete training (provided by Lead Entities) and use the Social Care Network IT platform
More information on payment amounts and processes can be shared by your regional Lead Entity.
Additional Information for Behavioral Health Care and other Providers
Health care providers are a key partner in the Social Care Network program, which aims to increase integration of physical health, behavioral health, and services that address health-related social needs. Coordinating these aspects of a Member's care is foundational to New York State's health equity goals. Please review the SCN: Introduction for Health Care Providers Guide (PDF).
Health care providers, including physical and behavioral health, can participate in the Social Care Network program in many ways:
- Talk to Medicaid patients about Social Care Networks and the services that may be available to them across nutrition, housing, transportation, and navigation supports; Lead Entities may share factsheets and other informational material that can be distributed via your offices
- Share contact information for a regional Lead Entity
- Conduct screening for health-related social needs in Medicaid patients using the Accountable Health Communities Health-Related Social Needs Assessment in the domains of housing, utilities, nutrition, transportation, employment, education, and interpersonal safety.
Providers who join a Social Care Network may receive reimbursement for screening and navigation of Medicaid Members if using twelve questions from the Accountable Health Communities Health-Related Social Needs Assessment. To receive reimbursement, health care providers must:
- Be in contract with a Lead Entity (providers working across multiple regions may contract with multiple Lead Entities)
- Be able to submit the HRSN screening through the regional Qualified Entity to the Statewide Health Information Network OR use the Social Care Network IT platform.
- Remain in good standing with New York Medicaid
Reach out to the Lead Entity in your region(s) to learn more.
Services Funded Under Waiver
CBOs and providers can be reimbursed for delivering services described in a “HRSN Fee Schedule.” Each SCN has been issued a fee schedule for their region. While the rates vary, the number of hours that can be reimbursed for each service is the same statewide.
Below is a highly condensed summary of each eligible service and the corresponding hours that can be reimbursed for that service for the entire waiver period—January 1, 2025 through March 31, 2027.
For instance, conducting the health-related social needs screening (Service Type: 0. Screening) would earn the provider 30 minutes of billable service. In New York City, this would equal $35. This service can only be delivered twice during the waiver period.
Service Type: 0 Screening
(Accountable Health Care HRSN Screening Tool below)
Capped at 30 minutes for the waiver period. A second screening may be authorized following a “major life event.”
Each Medicaid Member will receive a screening annually or on an as-needed basis due to a major life event.
- Conduct HRSN assessment using the Screening Tool.
- Enter responses into SCN IT Platform.
Service Type: 1.1 Navigation
Maximum of two hours (one hour after each screening) for waiver period.
Link non-eligible Medicaid Members to local benefits and programs.
- Help members access federal, state, and local benefits.
- Work with members on eligibility and care coordination (phone, virtual, or in person).
- Document activities in the IT platform and care plan.
Service Type: 1.2 Enhanced HRSN Care Management
Maximum of five hours through waiver period
Link eligible Members to Enhanced HRSN Services
- Assess eligibility, manage referrals, and coordinate care.
- Arrange transportation and educate members about services.
- Follow up to ensure services meet members' needs.
- Document all actions in the IT platform and care plan.
2.1 – 2.2c capped overall at $10,000 for cost of work. No reimbursement for “Social Care Navigator” or other staff coordinating the work.
2.1 Home Accessibility and Safety Modifications
Limited adaptations to allow the Member to live independently. Services include general education on how to use and properly care for equipment.
2.2a Home Remediation Service: Mold and Pest Remediation
Services may include mold and pest remediation.
2.2b Home Remediation Service: Ventilation Improving Systems
Repairs or improvement of ventilation systems.
2.2c Home Remediation: Equipment Provision
Medically necessary mini refrigeration units as needed for medical treatment and prevention (e.g., insulin)
The services below refer to 2.2a – 2.2c
- The Social Care Navigator refers the member to a “dwelling assessment provider” to evaluate the home for necessary changes.
- The dwelling assessment provider creates a plan, called a Scope of Work (SOW).
- The Social Care Navigator reviews the SOW, approves the needed services, and sends it to a service provider, making sure it stays within the budget limits.
- If the project costs more than $2,000, the provider must get at least three bids to ensure fair pricing.
- After bids are finalized, the provider or subcontractor starts the approved modifications.
2.3a Asthma Remediation: Self-Management Education
Maximum four hours in-person, two hours virtual for waiver period
Health education to expand asthma knowledge.
- Follow national asthma guidelines and focus on working together for asthma care.
- Services must be provided by qualified professionals.
- At least two in-person visits (one at the start and one at the end) must be done at the recipient’s home.
2.3b Asthma Remediation and Supportive Products
Cost-based, up to cap of $8,000
Services to remove indoor allergens and supply products to reduce asthma triggers. Asthma remediation contractors must hold appropriate licenses.
- The Social Care Navigator refers members to an Asthma Remediation Provider to assess their home for changes needed to reduce asthma triggers and improve indoor air quality.
- The provider creates a Scope of Work (SOW) with recommended services, costs, and administrative fees.
- The Social Care Navigator reviews the SOW, approves services, and refers it for execution, ensuring it stays within budget limits.
- For projects over $2,000, at least three bids must be collected, and the lowest qualified bid selected.
2.4 Medical Respite
Per diem: $245 - $388 up to 90 days per year
Temporary residential care for unstably housed Members who do not need to be hospitalized but require health care services.
- Short-term pre-procedure care and post hospitalization care by NYS-certified Medical Respite Programs.
- Must also offer transitional supports to secure stable housing and Enhanced HRSN services prior to the Member’s discharge.
2.5 Rent / Temporary Housing
Per unit per month, limited to 6 months (rates vary per region)
Rent / Temporary Housing includes payment for rent and/or short-term, temporary stays for up to six months.
- Services should be delivered by contracted experienced community-based providers and are registered as a 501(c)(3) or 501(c)(4) non-profit organization
- Contracted rent / temporary housing services may be performed by for-profit organizations at the SCN Lead Entity’s discretion.
2.6a Utility Setup - Activation Expenses
Cost-based, up to cap, one time, up to $350
Assistance with setting up utility services in Member’s new community living setting.
- Utility costs are limited to households receiving rent assistance / temporary housing
2.6b Utility Setup – Back Payment
Up to capped amount, one time: $4,566
Covers costs of back payments to secure and maintain utility service.
- Utility costs are limited to households receiving rent assistance / temporary housing
2.6c Utility Assistance
Cost-based, up to cap per month $761
Expenses for the following types of utility payments: gas/oil, electric, water, sewage, garbage, internet and phone (inclusive of landline and cell phone)
- Utility costs are limited to households receiving rent assistance / temporary housing
2.7 Pre-tenancy Services
Maximum 6 hours through waiver period
Assist with searching for rentals and contacting apartments, application process, negotiating lease agreements, and preparing for and attending tenant interviews.
- Services should be delivered by contracted experienced community-based providers and are registered as a 501(c)(3) or 501(c)(4) non-profit organization
- Contracted rent / temporary housing services may be performed by for-profit organizations at the SCN Lead Entity’s discretion.
2.8a Community Transitional Supports (CTS)
Cost-based, up to capped amount. (rates vary per region)
Assistance with the set-up of the new housing unit to ensure that it meets the Member’s needs.
- Included supports: deposit, utility activation fees, movers, and relocation expenses, pest eradication, pantry stocking (limited to a max of 30 days of food), household goods, and furniture.
2.8b CTS Broker's Fee
Cost-based, SCN-level cap.
2.9 Tenancy Sustaining Services
Maximum six hours through waiver period
Providing tenant rights education and eviction prevention services.
- Linking to free or affordable legal services.
- Assist in establishing a bank account and paying bills.
- Assistance in securing entitlements.
- Understanding and meeting the obligations of tenancy.
- Address behaviors that may jeopardize housing.
- Help resolve disputes with landlords and/or neighbors.
- Assist with housing recertification processes.
2.10 Housing Transition and Navigation Services
Maximum of four hours through waiver period
Services to assist with an eligible Member's transition into a new home, including:
- Assist with the set-up of the new housing
- Connect Member to resources aiding with housing costs and other expenses;
- Review the living environment and collaborate with the relevant provider staff where the individual is institutionalized to ensure a seamless transition to the community.
3.1 Nutrition Counseling and Education
Maximum of at two hours through waiver period
- Nutrition counseling and education services, covering topics on healthy meal preparation and connecting Members with grocery budget resources
- Services must be provided by certified dietitians, nutritionists, or nurse dieticians.
- Providers should be knowledgeable about nutrition principles and methods to help members achieve food security and meet dietary needs.
- Providers must follow best practices for food safety and assess nutrition needs based on age, activity, and health conditions like diabetes or obesity.
- Assessments guide food planning, tailored counseling, and meal preparation advice.
- Counseling and education can be for individuals or groups, covering nutrition assessments, meal planning, and grocery shopping guidance
3.2 Medically Tailored or Clinically Appropriate Home Delivered Meals
$10 - $16 per meal, up to 6 months (or 11 months for high-risk pregnant / post-partum individuals). Possibility of re-authorization.
Meal plans tailored to the medical needs of the Member, approved by a Registered Dietitian Nutritionist (RDN) or Certified Dietitian Nutritionist (CDN). Meals must adhere to established nutrition guidelines.
- Service is limited to 3 meals per day and can only be delivered to a Member's home.
3.3 Medically Tailored or Nutritionally Appropriate Food Prescriptions
$97 - $146 per week, up to 6 months (or 11 months for high-risk pregnant / post-partum individuals). Possibility of re-authorization
Food prescriptions in the form of a nutrition voucher or food boxes.
- Vouchers and coupons may only be redeemed at food pharmacies, farmer's markets, mobile markets, and Community Supported Agriculture (CSA) subscriptions.
- Vouchers will have a stated dollar amount and will serve to provide 3 meals/day, 7 days/week.
3.4 Fresh Produce and Non-perishable Groceries
$30 - $78 per week, up to 6 months (or 11 months for high-risk pregnant / post-partum individuals). Possibility of re-authorization
Pantry stocking of fresh produce and nonperishable groceries (excludes meat and dairy products). Fresh Produce and non-perishable groceries will serve as a nutritional supplement for up to 3 meals/day, 7 days/week.
3.5 Cooking Supplies: Kitchenware, Microwave, and Refrigerator
Global capped amount for each SCN (varies by region).
Cooking supplies that are necessary for meal preparation and nutritional welfare for a Member when not available through other programs, including microwave and refrigerator
- Should be provided by a CBO.
- Social Care Navigators to determine the specific needs of each Member
- Cooking supplies may include pots and pans, chef's knife, mixing bowls, cooking utensils, cutting board, eating utensils, plates, bowls, glassware, silverware, can opener and colander.
- The cost of a microwave and refrigerator can also be covered.
4.1 Transportation
Up to 6 months, with global capped amount for each SCN (varies by region).
Transportation services to Enhanced HRSN Services and activities. Transportation services may include taxi/livery, rideshare, or public transportation
Examples of eligible services or activities, include but not limited to:
- Housing appointments;
- Housing court (eviction prevention);
- Local Department of Motor Vehicles appointments;
- Employment interviews;
- Education and support for chronic conditions;
- Court, probation, parole, and order of protection-related appointments;
- Childcare / Parenting classes; and
- Food pharmacies, farmer's markets, mobile markets.
The Social Care Navigator will determine the most cost-effective and appropriate mode of transportation.
View the Screening Questionnaire
Living Situation
- What is your living situation today?
- I have a steady place to live.
- I have a place to live today, but I am worried about losing it in the future.
- I do not have a steady place to live (I am temporarily staying with others, in a hotel, in a shelter, living outside on the street, on a beach, in a car, abandoned building, bus or train station, or in a park).
- Member declined to answer.
- Think about the place where you live. Do you have problems with any of the following? (Choose all that apply):
- Pests such as bugs, ants, or mice
- Mold
- Lead paint or pipes
- Lack of heat
- Oven or stove not working
- Smoke detectors missing or not working
- Water leaks
- None of the above
- Member declined to answer.
Food
- Within the past 12 months, you worried that your food would run out before you got money to buy more.
- Often true
- Sometimes true
- Never true
- Member declined to answer.
- Within the past 12 months, the food you bought just didn't last and you didn't have money to get more.
- Often true
- Sometimes true
- Never true
- Member declined to answer.
Transportation
- In the past 12 months, has lack of reliable transportation kept you from medical appointments, meetings, work, or from getting things needed for daily living?
- Yes
- No
- Member declined to answer.
Utilities
- In the past 12 months has the electric, gas, oil, or water company threatened to shut off services in your home?
- Yes
- No
- Already shut off
- Member declined to answer.
Safety
- How often does anyone, including family and friends, physically hurt you?
- Never (0)
- Rarely (1)
- Sometimes (2)
- Fairly often (3)
- Frequently (4)
- Member declined to answer.
- How often does anyone, including family and friends, insult or talk down to you?
- Never (0)
- Rarely (1)
- Sometimes (2)
- Fairly often (3)
- Frequently (4)
- Member declined to answer.
- How often does anyone, including family and friends, threaten you with harm?
- Never (0)
- Rarely (1)
- Sometimes (2)
- Fairly often (3)
- Frequently (4)
- Member declined to answer.
- How often does anyone, including family and friends, scream or curse at you?
- Never (0)
- Rarely (1)
- Sometimes (2)
- Fairly often (3)
- Frequently (4)
- Member declined to answer.
A score of 11 or more when the numerical values for answers to questions 7-10 are added shows that the person might not be safe.
Career Pathways Training Program
The Career Pathways Training (CPT) Program is an education and training program that was authorized under New York's 1115 Demonstration Waiver, as part of the New York Health Equity Reform (NYHER) waiver amendment (you can find New York's Special Terms and Conditions here). This program is designed to create a reliable workforce pipeline to address workforce shortages by funding education and training for health, behavioral health and social care workers throughout New York State.
There are three approved categories of titles that participants of the program may pursue: nursing, professional technical, or frontline public health worker.
Learn More (DOH)

Care Compass Collaborative
Broome, Chenango, Delaware, Otsego, Tioga, Tompkins
Southern Tier
Mark Ropiecki Executive Director
Dawn Sculley, Director, SCN
Forward Leading IPA
Allegany, Cayuga, Chemung, Genesee, Livingston,Monroe, Ontario, Orleans, Schuyler, Seneca, Steuben, Wayne, Wyoming, Yates
Finger Lakes
Patty McMahon Executive Director
Lynette Thelen, Dir of Strategic Initiatives
Health and Welfare Council of Long Island
Nassau, Suffolk
Long Island
Lori Andrade Executive Vice President
Healthy Alliance Foundation Inc.
(1) Albany, Columbia, Greene, Rensselaer, Montgomery, Saratoga, Schenectady, Schoharie
(2) Cortland, Herkimer, Madison, Oneida, Onondaga, Oswego
(3) Clinton, Essex, Franklin, Fulton, Hamilton, Jefferson, Lewis, St. Lawrence, Warren, Washington
Capital Region, Central NY, North Country
Erica Coletti CEO
Hudson Valley Care Coalition, Inc.
Dutchess, Orange, Putnam, Rockland, Sullivan, Ulster, Westchester
Hudson Valley
Amie Parikh CEO
Public Health Solutions
Manhattan (4), Queens (5), Brooklyn (6)
Manhattan, Queens, Brooklyn
Zach Hennessey EVP
Keisha Barr, Senior Director, Healthcare Innovation
Staten Island Performing Provider System
Richmond
Staten Island
Joseph Conte Executive Director
Ashley Restaino, Network Membership
Morinsola Moroof-Mustapha, SCN Contact
Somos Healthcare Providers, Inc.
Bronx
Bronx
Mario J. Paredes CEO
Stephanie Duluc, EVP
Western New York Integrated Care Collaborative Inc.
Cattaraugus, Chautauqua, Erie, Niagara
Western NY
Nikki Kmicinski Executive Director